Effective Knowledge Management Implementation in 7 Steps
The amount of medical knowledge is presumed to double roughly every 73 days. But is your healthcare organization keeping up? In a complex industry bombarded with new research and rapid developments, even the most seasoned physicians struggle to retain everything relevant to delivering consistent, quality care.
Enter knowledge management systems (KMS)-the key to transforming scattered information into accessible insights that improve clinical outcomes for practitioners and patients.
Meet the Expert
Mical DeBrow is an accomplished healthcare leader and clinician with extensive expertise spanning pharma, healthcare payers and providers, and healthcare information technology.
» Learn how to harness information with knowledge management
Why Is a KMS So Important?
Think of a KMS as a smart assistant for your company's brain intent on breaking down knowledge silos. It gathers all the expertise, documents, and tips floating around, organizes them neatly, and makes them easily searchable for everyone.
An effective KMS also masters the act of balancing system-wide policies and department-specific protocols, alleviating a lot of confusion for healthcare staff. It's like having a Google for all your internal knowledge, boosting everyone's skills and saving time with every question answered.
Platforms like C8 Health provide a centralized and digitized hub for all point-of-care guidance and information, helping your healthcare team excel and achieve the best clinical outcomes.
1. Establish Clear Goals and Secure Buy-in From Key Stakeholders
The overarching goal behind implementing a KMS should focus on enhancing patient outcomes through integrating updated clinical information seamlessly into an automated workflow at the point of care.
In order to secure buy-in early on from stakeholders, consider:
- Bringing executives, physicians, nurse managers, risk management, and IT to the table for collaboration. Address concerns about costs and resources.
- Defining success metrics that align with larger organizational goals like reduced adverse events, better clinician workflow efficiency, and higher patient satisfaction. Using these factors to demonstrate ROI (return on investment) can help secure support.
To see how introducing knowledge management systems have impacted other healthcare organizations, download our latest case study.
2. Involve Frontline Clinician End-Users in Planning, Design, and Testing
IT systems fail when they don't bring clinical perspectives early enough into development. If physicians and nurses don't provide input, they will resent the system as an imposition on their workload and be less likely to utilize it correctly, if at all.
IT systems fail when they don't bring clinical perspectives early enough into development. If physicians and nurses don't provide input, they will resent the system as an imposition on their workload.
Interview nurses, doctors, and technicians about current workflow pain points and information needs. Have working sessions to review prototypes and provide detailed feedback on usability. At the end of the day, the system design should make their jobs easier, not harder.
"Select tech-savvy nurse and physician champions from different units to participate throughout. Compensate them appropriately for time spent away from clinical duties."
3. Prioritize Usability, Accessibility, and Clear Value to Users
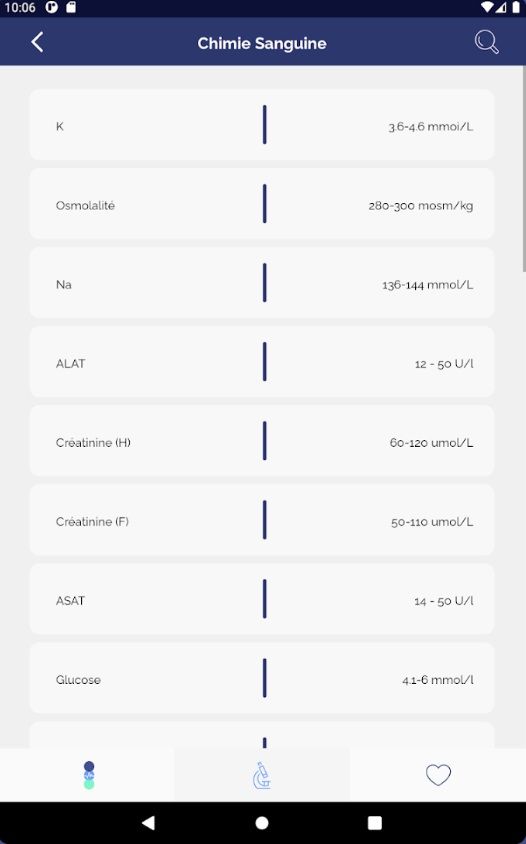
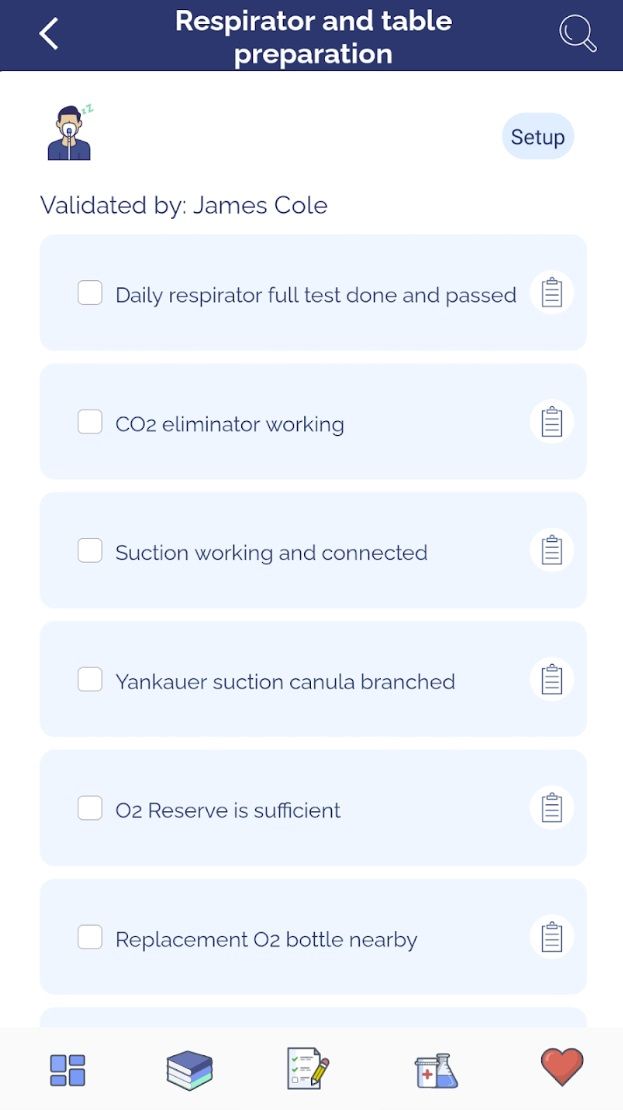
Simple and intuitive design is the key to securing users. Limit clicks, ensure workflow interoperability, and use clear language. The system should also be accessible on any device and seamlessly provide all the info clinicians need, such as security checks, procedures and protocols, and medication dosages.
Here's an example of effective knowledge management with C8's handy mobile app:
» Learn more about mobile technology in healthcare
4. Invest Heavily in End-User Training and Education
Evidence shows relying solely on classroom-based system training instead of simulation-based learning often fails to appropriately equip nurses with real-world system competency and familiarity.
To drive adoption when rolling out new technologies, organizations should budget additional funds to facilitate hands-on training. This allows each frontline nursing staff member at least 8 hours of hands-on time to practice live workflows and system functionality.
Additional support like supplemental eLearning courses, quick reference guide materials, video tutorials, and ongoing training updates as functionality evolves or new hires onboard further reinforce competence.
» Find out how to optimize staff onboarding with AI
5. Respond Rapidly to Address User Feedback Issues
Expect challenges as clinicians adjust workflows to use the system and have IT admins continuously gather user feedback to improve the experience.
Helpdesk call logs should be reviewed for trending issues, and bug fixes and enhancements must be prioritized in regular update cycles. User suggestions and challenges can be featured in newsletters or forums.
6. Track Relevant Metrics Pre- and Post-launch
Implementing new health technologies often focuses heavily on technical metrics like uptime, storage, and speed. Yet the core question remains: Does it improve patient outcomes? To find out, preprocessing and routine outcome data collection are important practices.
In an industry centered on patient care, technical gains must translate into real-life healing. Otherwise, the investments never fulfill their purpose. Tracking quantitative outcomes and experiences connects digital accomplishments to what matters most.
» Discover the ease of patient care with knowledge management
7. Publicize Success Stories to Recognize Contributions
Behind clinical metrics sit real individuals whose care journeys bend in new directions thanks to technology modernization efforts. Quantifiable safety improvements and outcome gains lack meaning if the people impacted feel otherwise.
Stats show progress and stories spur it further. Blending both elements cements technology's role in improving clinical outcomes and can keep clinicians and IT admins eager to continue improving.
Dr. Daniel Katz (Vice Chair of Education, Department of Anesthesia, Mount Sinai) shares his experience of how efficient knowledge management has boosted patient care:
Knowledge Management: A Vital Prescription for Healthcare
Knowledge management should be core to any healthcare organization seeking to raise the bar on patient care. By creating interconnected systems that surface insights, preserve institutional knowledge, and promote consistent best practices, care teams access an always-available playbook to make confident and informed decisions.
The end result is demonstrated in key metrics: refined onboarding, reduced errors, boosted guidelines adherence, increased research productivity, and elevated patient satisfaction from reliable, quality treatment.