6 Effective Strategies for Reducing Physician Burnout
Physician burnout results in staffing shortages and declining patient care. See how a multi-pronged approach empowers doctors, reduces workloads, and fosters well-being.


Medical Doctor Expertise Clinical Research, Medical Peer Reviewer and Independent Medical Evaluator, Knowledge management, Patient care Education Ross University School of Medicine- Doctor of Medicine (MD), Medicine, Florida State University College of Medicine- Doctor of Medicine (M.D.), Internal...
See Full BioLearn about our
Editorial PolicyPublished June 25, 2024.
Exhaustion is just the tip of the iceberg. According to a survey published in Mayo Clinic Proceedings, nearly 63% of physicians report at least one sign of burnout. To make matters worse, only 30% of them are satisfied with their work-life balance.
If it persists, this state can lead to depression, anxiety, and even suicidal thoughts. The good news is that there are ways to reduce it. By addressing the root causes and creating a more supportive work environment, we can ensure a healthier future for doctors and patients.
Meet the Expert
Zachary Gross, MD, is an internal medicine physician with expertise in clinical practice, pharmacovigilance, medical monitoring, and healthcare consulting.
Access Clinical Resources: Unite your department's knowledge on any device.
Manage Your Knowledge: Easily create, maintain, and update clinical resources.
Integrate Your Workflows: Deliver content directly to the point-of-care.
Collaborate and Communicate: Share knowledge and communicate across medical institutions.
Analyze Your Data: Track clinician engagement with custom insights.
» Check out innovative approaches for driving operational efficiency
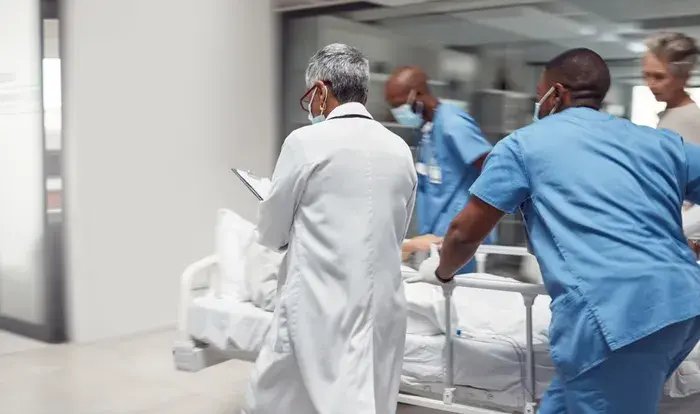
The Significant Cost of Burnout
When physicians quit, they create a shortage. This puts additional strain on the remaining staff, who may have to take on extra patients. The cycle leads to longer wait times, reduced quality of care, and increased workload.
With fewer employees, hospitals need to limit the number of new patients they can treat or even turn them away. This becomes a roadblock that prevents access to care in the community.
» Learn how C8 Health simplifies onboarding for new staff
1. Encourage Decision-Making
Healthcare systems and practices often dictate physician schedules based on case volumes, staffing, and operational demands. These factors may be outside of their control and impact their environment.
Studies show that hospitals that empower their doctors with decision-making and resources might improve overall performance. To encourage them, healthcare facilities can let them select what to prioritize for better work-life balance and reduced burnout.
For example, they could choose options for part-time employment, compressed workweeks, or evening or weekend hours to accommodate personal needs. If they decide to spend more time with each patient, they can effectively diagnose and develop treatment plans to increase care quality.
» Use AI and technology for innovative patient care
2. Rethink Reimbursement
The current fee-for-service model incentivizes physicians to see many patients daily, reducing the quality of care for each visit. Most current reimbursement metrics are surrogate markers-they stand in for the ideal outcome we care about.
In healthcare, it could reduce the risk of complications or improve long-term health and overall well-being. The problem is this method captures only part of the picture.
For example, you might see a person's improved blood pressure-but not if they're following the prescription. A fair system should account for factors like these to avoid penalizing doctors for details out of their control.
» Want to boost patient care? Efficient knowledge management can help
3. Improve Knowledge Sharing
Many factors can disrupt treatment plans. Some of them are the complexity of insurance company plans, limited medication coverage, and frequent changes to guidelines and clinical best practices.
Standardized protocols across care systems, a focus on cost-effectiveness for impactful medications, and a streamlined appeals process can offer some relief. But, improved information sharing is essential for these solutions to work effectively.
Platforms like C8 Health can play a crucial role by ensuring the entire healthcare team can access the most relevant and up-to-date information and best practices.
Access to a centralized hub of up-to-date information empowers physicians to make more informed decisions about medications and treatment plans. This reduces uncertainty and second-guessing, leading to greater confidence and a sense of control over patient care.
Our latest report showcases the current state of knowledge management in hospitals across the United States, highlighting the impact that knowledge management platforms can have on patient outcomes. Download it today to learn more.
4. Lighten the Administrative Load
Studies have shown doctors spend as much as 8.7 hours/ week on administrative tasks like interacting with insurance companies. This pressure can reduce their time for patient consultations and overall care.
Note: The US healthcare system, with its complex regulations, is a significant contributor to this burden. Physicians in countries with single-payer systems typically have less paperwork.
To address the issue, hospitals need clear guidelines and templates for progress notes, referrals, and other documentation. The staff can then format and write quickly. They can also use dedicated staff to schedule appointments, pre-authorize requests, and send bills.
5. Prioritize Physician Well-being
Investing in wellness programs and creating a supportive work environment can help lighten the load and reduce expenses in the long run.
For example, you can try workshops on stress management techniques, such as mindfulness meditation, or yoga. They can equip physicians with the tools to cope with demanding workloads and reduce the chances of burnout.
Creating peer support groups or confidential mentoring initiatives also helps doctors connect with colleagues, share experiences, and build community.
6. Expand Access to Primary Care
Expanding access to primary care can address the strain on emergency rooms due to non-emergency cases. This can involve several strategies:
- Attracting more medical students through financial incentives
- Using telehealth consultations to improve convenience
- Implementing team-based models with nurse practitioners and physician assistants to extend the reach of physicians.
» Learn about why technology is important in healthcare
Empowering Physicians to Thrive
Physician burnout is a complex issue with far-reaching consequences. It affects doctors' well-being and jeopardizes the quality of care patients receive. The good news is that there are solutions.
By providing mobile access to best practices and searchable content, C8 Health reduces wasted time searching for information. Automatic updates and push notifications ensure doctors are constantly working with the latest guidelines, empowering them to make informed decisions quickly
Additionally, C8 Health simplifies onboarding for new staff, helping them gain confidence and contribute more effectively, potentially reducing the workload for existing physicians. This focus on streamlined workflows can create a more supportive work environment and reduce physician burnout.