Staff Wellness: Ways to Keep Your Staff Healthy and Productive
Employees are feeling burnt out, stressed, and disengaged, leading to decreased productivity, higher turnover rates, and a negative company culture.
The relentless pace of work-combined with increasing demands and pressures-is taking a toll on employees' physical and mental health. Traditional wellness programs for staff often fall short, failing to address the root causes of workplace stress and burnout.
It's time to revolutionize workplace wellness. We've prepared wellness ideas for your staff so you can create a thriving and supportive work environment.
» Reduce paperwork and boost staff wellness with a knowledge management system
Challenges of Healthcare Wellness
Doctors and nurses work in a high-pressure environment. They face physical, emotional, and mental challenges every day. Even though 83% of hospitals have wellness programs, one in three healthcare workers still feel burned out. [1]
Healthcare professionals often grapple with the following:
- Intense Pressure: Doctors and nurses make life-or-death choices every day. The persistent pressure can be stressful and lead to burnout. [2]
- Emotional Toll of Patient Care: Caring for patients is emotionally draining. Doctors and nurses often witness their suffering and have tough conversations with their families. [3]
- Long and irregular hours: Working long, irregular hours can mess with your staff's sleep, make them tired all the time, and make it hard to balance their work and personal life. [4]
- Increased Risk: Healthcare workers often come into contact with germs and experience upsetting situations. Constantly dealing with this can lead to anxiety, fear, and even health problems. [5]
- Rapid Changes: Healthcare is constantly evolving. There are new procedures to learn and do all the time. This can be really tough and make people feel unsure of themselves.
- Overwhelming workload: According to a systematic review, a higher nursing workload was associated with increased patient mortality and adverse events. [6]
» Discover approaches that help reduce burnout in healthcare
The Wellness-Productivity Connection
Studies have shown that happy and healthy workers are more productive. This is especially important in healthcare, where patients' lives depend on it. [7]
When healthcare workers are well-rested and feel good, they're less likely to make medical errors. This makes patients happier and safer. By taking good care of staff, we also help them work better together. Happy teams are more productive and efficient.
While technology has entered healthcare, much of it hasn't been designed with healthcare providers in mind. Many new tools and apps focus on patients, not doctors and nurses. We need more technology specifically for healthcare professionals.
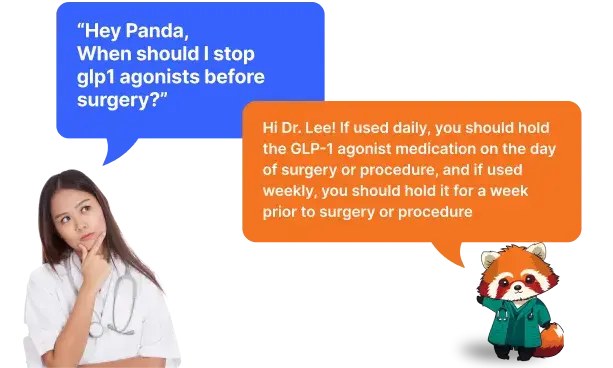
- Without a digitized system, it's challenging to locate specific protocols.
- Even when you find them, there's the matter of their validity. Can you trust a protocol from 2002? Is it updated? Is it still relevant?
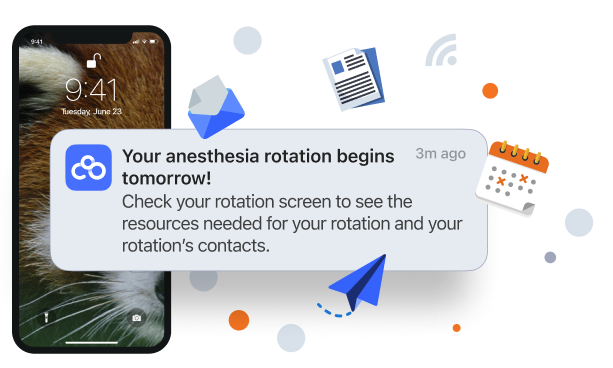
That's why we created C8 Health: to close the knowledge gap in healthcare. You can store all your organizational know-how in one place and make it available to your staff. They can save time searching for information by asking our AI assistant questions.
Wellness Ideas for Preventing Staff Burnout
Hospitals can play a big role in helping them stay healthy and happy, even though doctors are responsible for their well-being.
Here are some things you can do:
1. Detailed Wellness Program for Staff
Wellness programs can do wonders for your staff. A study found that while a workplace wellness program can improve overall health and productivity. Specifically, the program increased the number of employees who reported engaging in physical activities and managing their weight. [8]
» Learn how to calculate your turnover rate
2. Mental Health Support
Many hospitals now understand that working in healthcare takes its toll. They're offering private counseling and support groups where staff can talk to professionals or other workers who know what they're going through.
A systematic review examined studies involving healthcare workers on the front lines of COVID-19 care. [9] Interventions were primarily online or digital and generally showed positive outcomes in terms of reducing stress and improving healthy support-seeking behaviors.
So, help your employees take care of their mental health. Offer private counseling, support groups for tough times, and workshops to help them cope better. Make sure they have quiet places to relax and recharge.
» Discover crucial hospital quality metrics
3. Work-Life Balance Initiatives
Healthcare workers are feeling increasingly stressed and overwhelmed due to their demanding jobs. A recent study showed that their job satisfaction and personal life balance vary greatly depending on their specific role and workplace environment. [10]
Additionally, the study found that a positive work-life balance culture within a healthcare setting can lead to better teamwork, safer practices, and reduced burnout among staff.
You should introduce flexible scheduling options to promote work-life balance. Try compressed workweeks and flexible working hours. Optimizing shift schedules can also help prevent burnout. Analyze staffing patterns and distribute shifts fairly so everyone gets equal rest.
Finally, you can encourage vacation time to help staff recharge and return to work feeling refreshed. Providing childcare support, such as on-site facilities or subsidies, can also help with stress management for employees with children, allowing them to better balance their work hours and personal lives.
» Learn about the advantages of collaboration in healthcare
4. Professional Development and Growth
A study found that continuing education programs can help improve the skills and knowledge of healthcare workers in long-term care facilities. [11] These programs are especially beneficial for learning about dementia care and reducing the use of restraints.
To put this idea to use, implement mentorship programs. You can pair experienced staff members with newer colleagues, encouraging knowledge-sharing, skill development, and personal growth.
Additionally, you can offer clear career progression paths to motivate staff and give them a sense of purpose and direction. You can also offer regular skill development workshops and training sessions to keep staff updated with the latest advancements in healthcare.
» Explore tips on training healthcare employees
5. Workload Management
Nurse leaders in public healthcare settings often feel overwhelmed by their workload. A study found that they frequently work overtime, delegate tasks, and request additional staff to manage their heavy responsibilities. [12]
The perception of workload varies depending on factors like the number of staff and their characteristics. This suggests that staffing decisions should consider not only the quantity of staff but also their skills and experience.
Regularly assess staffing levels and adjust as needed to prevent overwork. Implement task-sharing and delegation protocols to distribute workload effectively across the team. Use data analytics to predict busy periods and staff accordingly, avoiding understaffing during peak times.
Provide administrative support to employees to reduce non-clinical workload, allowing healthcare professionals to focus more on patient care and less on paperwork.
» Implement a knowledge management system to reduce workloads
Creating a Culture of Care
The connection between staff wellness and operational efficiency in healthcare is undeniable. It's a complex issue that requires recognition, support, and the right tools.
The experiences shared here shed light on the challenges faced in the healthcare industry and how technology, when designed with clinicians in mind, can play a pivotal role in improving staff wellness and ultimately enhancing patient care.
» Boost staff wellness with a user-friendly knowledge management system
References:
- "Health worker mental health crisis," Centers for Disease Control and Prevention, Oct. 24, 2023. Available: https://www.cdc.gov/vitalsigns/health-worker-mental-health/index.html
- M. F. Jiménez-Herrera, M. Llauradó-Serra, S. Acebedo-Urdiales, L. Bazo-Hernández, I. Font-Jiménez, and C. Axelsson, "Emotions and feelings in critical and emergency caring situations: a qualitative study," BMC Nursing, vol. 19, no. 1, Jul. 2020, doi: 10.1186/s12912-020-00438-6. Available: https://doi.org/10.1186/s12912-020-00438-6
- E. Nena, M. Katsaouni, P. Steiropoulos, E. Theodorou, T. Constantinidis, and G. Tripsianis, "Effect of shift work on sleep, health, and quality of life of health-care workers," Indian Journal of Occupational and Environmental Medicine, vol. 22, no. 1, p. 29, Jan. 2018, doi: 10.4103/ijoem.ijoem_4_18. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5932908/
- C. C. Caruso, "Negative impacts of shiftwork and long work hours," Rehabilitation Nursing, vol. 39, no. 1, pp. 16-25, Jan. 2014, doi: 10.1002/rnj.107. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4629843/
- S. Acke, S. Couvreur, W. M. Bramer, M.-N. Schmickler, A. De Schryver, and J. A. Haagsma, "Global infectious disease risks associated with occupational exposure among non-healthcare workers: a systematic review of the literature," Occupational and Environmental Medicine, vol. 79, no. 1, pp. 63-71, May 2021, doi: 10.1136/oemed-2020-107164. Available: https://pubmed.ncbi.nlm.nih.gov/34035182/
- P. Ross, B. Howard, D. Ilic, J. Watterson, and C. L. Hodgson, "Nursing workload and patient‐focused outcomes in intensive care: A systematic review," Nursing and Health Sciences, vol. 25, no. 4, pp. 497-515, Oct. 2023, doi: 10.1111/nhs.13052. Available: https://pubmed.ncbi.nlm.nih.gov/37784243/
- C. S. Bellet, J.-E. De Neve, and G. Ward, "Does employee happiness have an impact on productivity?," Management Science, vol. 70, no. 3, pp. 1656-1679, Mar. 2024, doi: 10.1287/mnsc.2023.4766. Available: https://doi.org/10.1287/mnsc.2023.4766
- Z. Song and K. Baicker, "Effect of a workplace wellness program on employee health and economic outcomes," JAMA, vol. 321, no. 15, p. 1491, Apr. 2019, doi: 10.1001/jama.2019.3307. Available: https://pubmed.ncbi.nlm.nih.gov/30990549/
- M. Härkänen et al., "The impact of emotional support on healthcare workers and students coping with COVID-19, and other SARS-CoV pandemics - a mixed-methods systematic review," BMC Health Services Research, vol. 23, no. 1, Jul. 2023, doi: 10.1186/s12913-023-09744-6. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10339499/
- S. P. Schwartz et al., "Work-life balance behaviours cluster in work settings and relate to burnout and safety culture: a cross-sectional survey analysis," BMJ Quality & Safety, vol. 28, no. 2, pp. 142-150, Oct. 2018, doi: 10.1136/bmjqs-2018-007933. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6365921/
- M. Gkioka, J. Schneider, A. Kruse, M. Tsolaki, D. Moraitou, and B. Teichmann, "Evaluation and Effectiveness of Dementia Staff Training Programs in General Hospital Settings: A Narrative Synthesis with Holton's Three-Level Model Applied," Journal of Alzheimer S Disease, vol. 78, no. 3, pp. 1089-1108, Nov. 2020, doi: 10.3233/jad-200741. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7739966/
- M. Miller and J. Hemberg, "Nurse leaders' perceptions of workload and task distribution in public healthcare: A qualitative explorative study," Journal of Clinical Nursing, vol. 32, no. 13-14, pp. 3557-3567, Jun. 2022, doi: 10.1111/jocn.16428. Available: https://pubmed.ncbi.nlm.nih.gov/35773960/
Disclaimer: Our content serves informational purposes only and shouldn't replace the advice and services of qualified professionals. While we strive for accuracy, we cannot guarantee an entirely error-free experience. C8 Health will not be liable for any losses or damages resulting from the use of our content.