How to Identify Gaps in Healthcare and Close Them Effectively
Why do experts worldwide invest time and money in research? To discover evidence that supports treatment. From their findings, policymakers create guidelines that inspire protocols of hospitals everywhere.
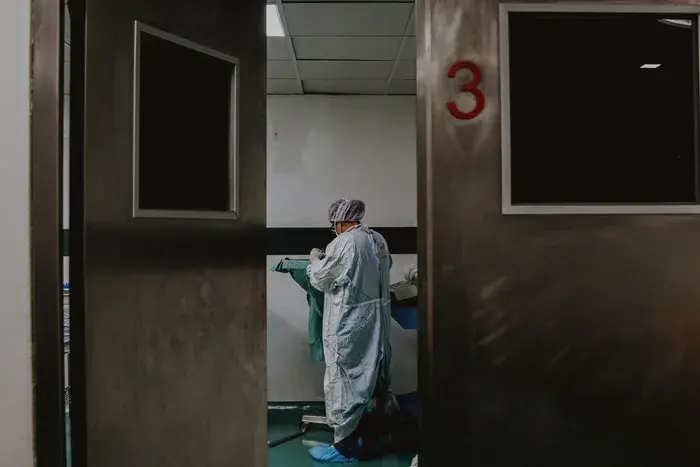
During COVID-19, guidelines for surgery and testing became an issue. Medical staff were at a 10x more risk of exposure, especially when giving anesthesia. [1] The lack of well-defined policies confused clinicians.
The result? Many people canceled surgery, harming hospital finances and delaying care. Below, we take a look at how you can find these gaps in healthcare and close them.
» Close gaps in your healthcare facility with knowledge management
What Are Gaps in Healthcare?
A gap is when the care a patient receives falls short of the recommended standard. These mistakes are due to several factors:
- Insufficient health insurance, access to care, finances, or understanding of health information.
- Inexperienced providers, limited equipment, staff shortages, and appointment time constraints.
- Inefficient communication between departments, fragmented care delivery, and coordination within the hospital.
Examples of Care Gaps:
- Missing cancer screenings or colonoscopies.
- Ignoring medication instructions for diabetes or high blood pressure.
- Skipping follow-up appointments after a hospital stay.
» Reduce medical errors and improve patient safety
Why Are They Important?
Addressing these gaps is critical because it can:
- Improve patient outcomes by catching problems early and managing chronic conditions effectively.
- Ensure access to care for everyone.
- Reduce healthcare costs by preventing complications that require more expensive interventions.
» Learn why quality improvement in healthcare is important
How to Identify Gaps in Healthcare
Finding where patient care falls short is crucial if you're to improve health outcomes. For that, you need a strategic method. Here's what you can do:
1. Failure Mode and Effects Analysis (FMEA)
Lastly, you can use FMEA to find the root causes of issues. [2] Let's say you want to improve diabetes management and prevent complications. Here's how you would do it:
- Define the Process: Medication management, blood glucose monitoring, and follow-up appointments.
- Find Failure Modes: Patients not following any of the defined processes.
- Check for Effects: Increased risk of hyperglycemia, hypoglycemia, heart disease, etc.
- Assess severity, occurrence, and detection: Assign ratings to each failure mode based on their potential severity, the likelihood of occurrence, and the ease of detection.
» Discover the most important hospital quality metrics
2. Hospital Consumer Assessment of Healthcare Providers (HCAHPS) Scores
We can also use HCAHPS scores to measure how patients feel over time and compare it to what patients tell us directly. [3] Let's say that a hospital consistently receives low scores on the "communication with doctors" HCAHPS question.
This shows a need for:
- Better training for physicians on communication skills
- Simpler communication protocols within the care team
- Greater patient empowerment through education on how to effectively communicate with their providers.
You can also compare your HCAHPS to other hospitals to find best practices and track improvement efforts over time.
Looking at data is helpful for understanding issues, but you should also listen to what patients are saying. Combining qualitative and quantitative insights helps you look at the problem from more angles.
» Make data-driven decisions for your healthcare facility
Patient Opinions
Understanding how patients feel about their care is crucial for finding gaps in healthcare services. You can learn about this by asking them directly through surveys, group discussions, and one-on-one talks.
Another way is to look at social media and patient experience portals. Just make sure your group. Separate patients based on age, sex, race, and income level to get a nuanced perspective.
You should also analyze the feedback if you're to turn it into useful information. Why? Because it'll help you decide what to do next. Special methods like sentiment and thematic analysis can help you find vital patterns in the data and share them with staff.
» Improve patient care with efficient knowledge management
Strategies for Gap Closing
1. Invest in Centralized Knowledge Management
Groups like the American College of Cardiology and American Heart Association create guidelines, but these are just suggestions. Each hospital has its own rules. A major problem in sharing knowledge is making sure doctors know about and follow them. But how would you do it?
A knowledge management system can help you close gaps in care by delivering information to the right clinician at the right time. Here's what you get by using one in your organization:
- Instant access to information in a centralized repository, including clinical, practical, and administrative knowledge.
- Frequent updates that inform all users.
- Diverse content formats for mobile and desktop use.
- Advanced analytics to check how clinicians use your content.
Want to Prevent Patient Harm During Inpatient Care?
Unite all your guidelines and make them easily accessible. C8 Health's natural language querying and AI assistant ensure quick access to crucial clinical data.
Find out why we're trusted by the leading organizations worldwide, such as the Society for Obstetric Anesthesia and Perinatology.
2. Educate and Engage Patients
People who are more involved in managing their condition have better health. [4] Studies show that they are better at finding and using health information to improve their health. This is what we call "patient activation." [5]
Healthcare providers should communicate clearly and involve patients in decision-making. It can lead to better health outcomes and satisfaction.
» Try best practices for knowledge management to boost patient care
3. Research Social Determinants of Health (SDOHs)
SDOHs are powerful factors in determining overall health outcomes. [6] Healthcare systems can reduce gaps in care and improve the well-being of entire communities by addressing these underlying issues.
Here's how SDOH can help close care gaps:
- Identifying vulnerable populations: Healthcare providers can pinpoint areas with higher health risks and allocate resources by understanding the social factors that impact a community.
- Addressing root causes: SDOH interventions tackle the fundamental reasons for health disparities, such as poverty, lack of education, and housing insecurity.
- Promoting preventive care: Patients are better equipped to prevent illness and manage chronic conditions.
- Building stronger communities: Oftentimes, addressing SDOH involves community partnerships, which can lead to better social cohesion and support networks.
» Upgrade your facility with the latest health information technology
Better Care Through Better Understanding
Finding and fixing problems in healthcare is crucial for improving patient safety and outcomes. We can find these issues by looking closely at patient data, asking them what they think, and working together as a team.
Once we know what's wrong, we can fix it by teaching patients, making sure care is smooth, and working with the community. If we do all these things and put patients first, everyone will get better care. Eager to get started?
» Close gaps in care with a knowledge management system
References:
- T. Dzinamarira et al., "Risk factors for COVID-19 infection among healthcare workers. A first report from a living Systematic review and meta-Analysis," Safety and Health at Work, vol. 13, no. 3, pp. 263-268, Sep. 2022, doi: 10.1016/j.shaw.2022.04.001. Available: https://pubmed.ncbi.nlm.nih.gov/35433073/
- S. M. M. El-Awady, "Overview of Failure Mode and Effects Analysis (FMEA): a patient safety tool," Global Journal on Quality and Safety in Healthcare, vol. 6, no. 1, pp. 24-26, Feb. 2023, doi: 10.36401/jqsh-23-x2. Available: https://pubmed.ncbi.nlm.nih.gov/37260856/
- "HCAHPS: Patients' Perspectives of Care Survey | CMS." Available: https://www.cms.gov/medicare/quality/initiatives/hospital-quality-initiative/hcahps-patients-perspectives-care-survey
- "Health literacy research and best practices," Centers for Disease Control and Prevention, Aug. 16, 2021. Available: https://www.cdc.gov/healthliteracy/researchevaluate/patient-engage.html
- J. H. Hibbard and J. Greene, "What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs," Health Affairs, vol. 32, no. 2, pp. 207-214, Feb. 2013, doi: 10.1377/hlthaff.2012.1061. Available: https://pubmed.ncbi.nlm.nih.gov/23381511/
- World Health Organization: WHO, "Social determinants of health," May 30, 2019. Available: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1
Disclaimer: Our content serves informational purposes only and shouldn't replace the advice and services of qualified professionals. While we strive for accuracy, we cannot guarantee an entirely error-free experience. C8 Health will not be liable for any losses or damages resulting from the use of our content.